ABSTRACT
Introduction: Botulinum neurotoxin A (BoNTA) has long been used as a therapeutic agent and has been widely accepted as a cosmetic agent in recent years. It can inhibit function and induce structural changes in skeletal muscle. Methods: Specimens of fresh dissected human masseter muscle were used to observe the ultrastructural changes that occurred at 6 and 12 months following BoNTA injection. Results: The findings observed were muscle fiber distortion, sarcomere shortening, mitochondrial vacuolar degeneration, glycogen accumulation, and H and M band disruption in the triad of tubules. At 12 months after injection, there was still evidence of degenerative changes in muscle ultrastructure, whereas most organelles exhibited a normal structure. Discussion: Profound ultrastructural and organelle disfiguring changes were observed after BoNTA injection into human masseter muscle. Most changes were transient, however, and were resolved by 12 months after injection.
Keywords
Botulinum toxin A, human masseter muscle, ultrastructuralchanges, electron microscope, mitochondria, sarcomere
Botulinum neurotoxin A (BoNTA) was first usedtherapeutically by local injection in 1980.1 Themechanism of action of BoNTA is inhibition of thesynaptic release of acetylcholine, thereby blockingneuromuscular transmission.2 A study of biochemicalchanges in neuromuscular junctions afterBoNTA injection illustrated its mechanism ofaction.3 General histologic and ultrastructuralchanges in muscle tissue after treatment have alsobeen studied.4–6 Because of difficulties with humantissue sampling, ultrastructural changes in humanstriated muscles after BoNTA injection have notbeen studied. This study examines specimens ofhuman masseter muscle by electron microscopy(EM) to assess their ultrastructural changes at differenttimes after BoNTA injection.
MATERIALS AND METHODS
This study was approved by the ethics committee of WeifangMedical University. After informed consent wasobtained, 9 Asian women with bilateral masseter musclehypertrophy (who planned to undergo partial removal ofthe masseter muscle to narrow the lower face at the PlasticSurgery Hospital of Weifang Medical University) were selectedas study participants. The ages of patients ranged from20 to 30 years. Three patients received local injections ofBoNTA in the masseter muscles bilaterally 6 months prior tosurgery, and 3 patients received injections 12 months prior tothe surgery. Three patients who did not receive local injectionsof BoNTA before masseter muscle removal were included ascontrols. The masseter muscles of all 9 patients were partiallyremoved bilaterally, and the specimens were immediately pretreatedin the operating room. In total, 18 specimens wereprocessed for EM. The BoNTA injected in the patients wasHengli BoNTA (Lanzhou Institute of Biological Products, LanzhouGansu Province, People’s Republic of China); a dose of50 units was used for the muscle on each side.
An appropriate amount of masseter muscle, as judgedby the patients’ surgeons, was removed from the patients viaan intraoral incision under general anesthesia. A 1-mm2fragment of muscle tissue was extracted from the fiber-richparts of the severed masseter muscle. The tissue fragmentwas immediately submerged in 2.5% glutaraldehyde fixationfluid and preserved at 4 8C. The specimens were processedfor EM by standard methods.7
An HL 7500 transmission electron microscope (Hitachi,Chiyoda, Japan) was used. Analysis of all specimens was performedby the same researcher.
RESULTS
Facial Contour
The width of the lower face startedto decrease 2–3 weeks after injection, and, by 4–6months postinjection, the width had decreased byapproximately 10%, as measured by CT scan. Thevolume of the muscle then began slowly toincrease, and, by 12 months postinjection, thewidth was 5% less than that before injection.
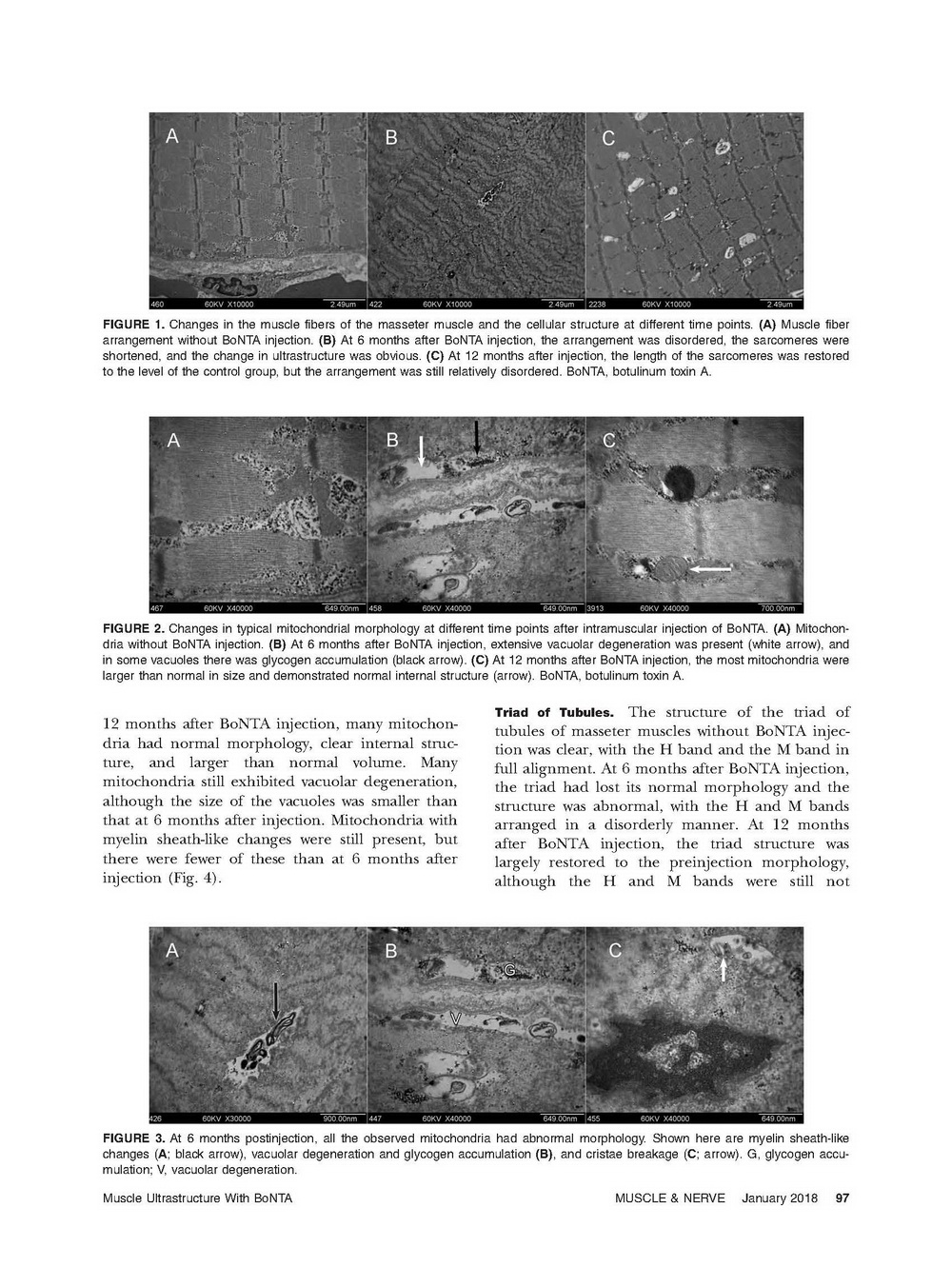
Muscle Fibers and Cellular Structure
The sarcomeresin the patients without BoNTA injectionwere aligned well and were of consistent length. Incontrast, the arrangement of masseter musclefibers at 6 months after BoNTA injection was verydistorted, the sarcomeres were shortened, and the change in ultrastructure was unequivocal. Thelength of the sarcomeres at 12 months after injectionwas restored to that of the control group, butthe arrangement was still relatively distorted, andthe ultrastructure was obviously different from thatin the control group (Fig. 1).
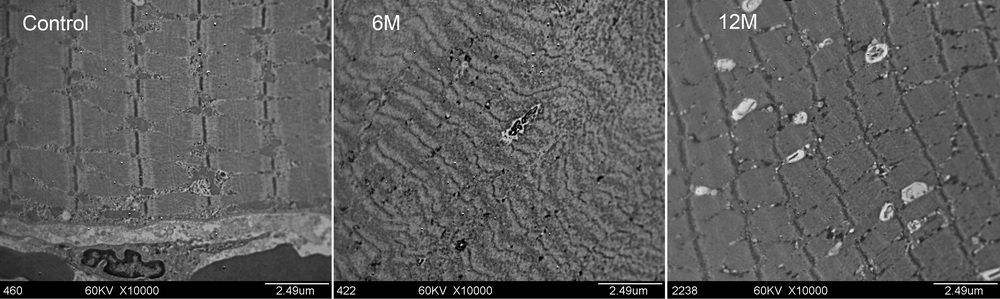
FIGURE 1. Changes in the muscle fibers of the masseter muscle and the cellular structure at different time points. (A) Muscle fiberarrangement without BoNTA injection. (B) At 6 months after BoNTA injection, the arrangement was disordered, the sarcomeres wereshortened, and the change in ultrastructure was obvious. (C) At 12 months after injection, the length of the sarcomeres was restoredto the level of the control group, but the arrangement was still relatively disordered. BoNTA, botulinum toxin A.
Mitochondria
It was difficult to observe normalmitochondrial structure in human massetermuscles at 6 months after BoNTA injectionbecause of extensive vacuolar degeneration, andsome vacuoles exhibited glycogen accumulation.Myelin sheath-like changes and cristae breakagewere evident in many mitochondria. (Figs. 2, 3). At 12 months after BoNTA injection, many mitochondriahad normal morphology, clear internal structure,and larger than normal volume. Manymitochondria still exhibited vacuolar degeneration,although the size of the vacuoles was smaller thanthat at 6 months after injection. Mitochondria withmyelin sheath-like changes were still present, butthere were fewer of these than at 6 months afterinjection (Fig. 4).

FIGURE 2. Changes in typical mitochondrial morphology at different time points after intramuscular injection of BoNTA. (A) Mitochondriawithout BoNTA injection. (B) At 6 months after BoNTA injection, extensive vacuolar degeneration was present (white arrow), andin some vacuoles there was glycogen accumulation (black arrow). (C) At 12 months after BoNTA injection, the most mitochondria werelarger than normal in size and demonstrated normal internal structure (arrow). BoNTA, botulinum toxin A.

FIGURE 3. At 6 months postinjection, all the observed mitochondria had abnormal morphology. Shown here are myelin sheath-likechanges (A; black arrow), vacuolar degeneration and glycogen accumulation (B), and cristae breakage (C; arrow). G, glycogen accumulation;V, vacuolar degeneration.

FIGURE 4. (A) Many mitochondria with normal morphology, clear internal structure, and larger than normal volume were observed at12 months after injection (arrow). Some mitochondria still exhibited myelin sheath-like changes (B; arrow) and vacuolar degeneration(C), but the number of mitochondria with abnormal morphology was significantly reduced compared with that at 6 months after injection.V, vacuolar degeneration.
Triad of Tubules
The structure of the triad oftubules of masseter muscles without BoNTA injectionwas clear, with the H band and the M band infull alignment. At 6 months after BoNTA injection,the triad had lost its normal morphology and thestructure was abnormal, with the H and M bandsarranged in a disorderly manner. At 12 monthsafter BoNTA injection, the triad structure waslargely restored to the preinjection morphology,although the H and M bands were still not completely aligned; the Z-line was mostly normal,and its basic structure could be identified (Fig. 5).

FIGURE 5. Changes in the triad of tubules at different times after BoNTA injection. (A) The structure of the triad of tubules withoutBoNTA injection was clear (arrow). (B) At 6 months after BoNTA injection, the triad had lost its normal morphology (arrow). (C) At 12months after injection, the triad structure was restored to the preinjection morphology (arrow). BoNTA, botulinum toxin A.
DISCUSSION
We investigated a total of 18 specimens from 9patients to observe the effect of BoNTA on theultrastructure of human masseter muscles andfound that the ultrastructure of this muscle wassubstantially changed after BoNTA injection. Thesechanges consisted of rearrangement of thesequence of muscle fibers (similar to the changesfollowing denervation by nerve section)8,9 andchanges to the structures of the nuclei and mitochondria.Vacuolar degeneration of mitochondriawas consistent with the mitochondrial ultrastructuralchanges in patients with mitochondrialencephalomyopathies,10 and increased glycogenaccumulation was consistent with the mitochondrialultrastructural changes in patients with mitochondrialmyopathy.11 We also observed thephenomenon of glycogen accumulation that wehad seen in patients with myasthenia gravis in ourother unpublished studies.
本文是原文的缩减版。原文于2018年1月8日发表在《肌肉与神经杂志》(Muscle and Nerve)第57卷第1期66-69页。
由于版权原因,恕文章后2页的内容不能列出。
下面是这篇文章的 Pubmed 查询结果及 SCI 收录情况。
References
1. Scott AB. Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery. J Pediatr Ophthalmol Strabismus 1980;17:21–25.
2. Baskaran P, Thyagarajan B. Acute and chronic effects of botulinum neurotoxin A on the mammalian neuromuscular junction. Muscle Nerve 2014;50:206–15.
3. Dressler D, Adib Saberi F. Botulinum toxin: mechanisms of action. Eur Neurol 2005;53:3–9.
4. Duchen LW. Changes in the electron microscopic structure of slow and fast skeletal muscle fibres of the mouse after the local injection of botulinum toxin. J Neurol Sci 1971;14:61–74.
5. Capra NF, Bernanke JM, Porter JD. Ultrastructural changes in the masseter muscle of Macaca fascicularis resulting from intramuscular injections of botulinum toxin type A. Arch Oral Biol 1991;36:827–836.
6. Hassan SM, Jennekens FG. Botulinum toxin-induced myopathy in the rat. Brain 1995;118(Pt 2):533–545.
7. Victor D, Caroline AS, Anders O. 2013. Muscle biopsy: a practical approach. Philadelphia: Saunders Elsevier.
8. Miledi R, Slater CR. Electron microscopic structure of denervated skeletal muscle. Proc R Soc Lond B Biol Sci 1969;174:253–269.
9. Bardosi A, Goebel H, Stennert E. The ultrastructure of normal and denervated human facial muscle. Plast Reconstr Surg 1987;79:171–176.
10. Debray FG, Seneca S, Gonce M, Vancampenhaut K, Bianchi E, Boemer F, et al. Mitochondrial encephalomyopathy with cytochrome c oxidase deficiency caused by a novel mutation in the MTCO1 gene. Mitochondrion 2014;17:101–105.
11. Jerusalem F, Angelini C, Engel AG, Groover RV. Mitochondria-lipidglycogen (MLG) disease of muscle. A morphologically regressive congenital myopathy. Arch Neurol 1973;29:162–169.